Learning all about the immune system
 Sunday, June 14, 2020 at 3:00PM
Sunday, June 14, 2020 at 3:00PM Happy readers of "Battle Robots of the Blood"!
 science communication
science communication Becoming a Scientist
Virus Fighter
Build a virus or fight a pandemic!
Maya's Marvellous Medicine
Battle Robots of the Blood
Just for Kids! All about Coronavirus
Learn about our spin-off, Aila Biotech!
 Sunday, June 14, 2020 at 3:00PM
Sunday, June 14, 2020 at 3:00PM Happy readers of "Battle Robots of the Blood"!
 Monday, June 8, 2020 at 9:47PM
Monday, June 8, 2020 at 9:47PM Coronavirus science simplified: number 6. This article in Nature Medicine looked at the amount of virus present in patients before and after they got symptoms. The data is clear: you can spread COVID19 before you actually get sick, so wear a mask! Read the original paper, or see the illustrated abstract by Tenmai.

 Wednesday, June 3, 2020 at 3:05PM
Wednesday, June 3, 2020 at 3:05PM This is a strange time for any workplace. People suddenly working from home, large changes in job duties, some people left without much to do while others are expected to manage whole new realms of bureaucracy while also continuing their full-time job. For us, as an immunology lab, this pandemic has an added dimension of peculiarity: our work is directly relevant to the ongoing situation.
 Looking back on how we dealt with the outbreak, we were ahead of the curve. We put in place strict social distancing and work-from-home measures well before our institutes / government did (and, I would argue as an immunologist, our lab rules were more science-based than those later imposed on us). We also started a public education program on COVID-19, with an interactive Virus Outbreak simulator, an illustrated series translating scientific articles into lay language and even released a kid's book explaining Coronavirus (with special thanks to lab members Dr Teresa Prezzemolo, Julika Neumann and Dr Mathijs Willemsen for translating this into different languages).
Looking back on how we dealt with the outbreak, we were ahead of the curve. We put in place strict social distancing and work-from-home measures well before our institutes / government did (and, I would argue as an immunologist, our lab rules were more science-based than those later imposed on us). We also started a public education program on COVID-19, with an interactive Virus Outbreak simulator, an illustrated series translating scientific articles into lay language and even released a kid's book explaining Coronavirus (with special thanks to lab members Dr Teresa Prezzemolo, Julika Neumann and Dr Mathijs Willemsen for translating this into different languages).
We also had lab members head back to the clinic to help with the capacity issues created by COVID-19. Dr Frederik Staels and Dr Erika Van Nieuwenhove suspended research to increase their clinical duties, and Dr Stephanie Humblet-Baron and Dr Mathijs Willemsen were on-call in case the system was overwhelmed.
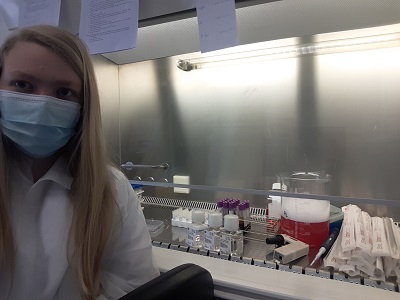 Silke Janssen, processing patient blood
Silke Janssen, processing patient blood
Our lab never completely shut-down though - we had important work that needed to be done. I'd like to call out Dr Susan Schlenner, Dr James Dooley and Dr Lubna Kouser who led the unglamorous but key administration on securing the safety of team members who had to be in the lab. Our Leuven lab was central to the processing of clinical COVID-19 samples. We usually think of clinical trials being run by MDs, but the work does not end after the blood is collected. I really want to call out the key contributions of Silke Janssens and Dr Teresa Prezzemolo. Without them, coming in all day, every day to process blood samples, clinical research of COVID-19 would have been crippled.
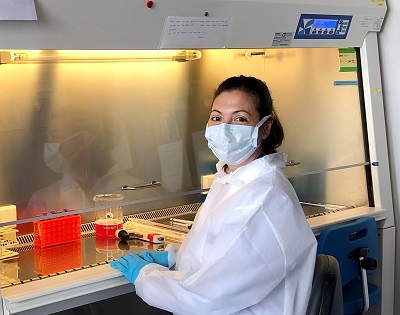 Dr Teresa Prezzemolo in the L2 labOur team, lead by Dr Stephanie Humblet-Baron, also analysed the samples prepared. We performed an ultra-high parameter analysis (far beyond state-of-the-art hospital diagnostics) of the T cell phenotype of COVID-19 patients: months of work from Dr Teresa Prezzemolo, Silke Janssens, Julika Neumann and Dr Mathijs Willemsen. Data analysis by Julika Neumann, Dr Carlos Roca, Dr Oliver Burton and Dr Stephanie Humblet-Baron identified a novel link between IL-10-producing Tregs and COVID-19 severity. We are now following this up to see if the link is useful as a biomarker or even is mechanistic in disease program. We have made our data an open resource (link), allowing other groups around the work to analyse our work. We are continuing to follow these patients and will soon have more and more information about why some patients remain completely healthy and others develop severe, even fatal, disease.
Dr Teresa Prezzemolo in the L2 labOur team, lead by Dr Stephanie Humblet-Baron, also analysed the samples prepared. We performed an ultra-high parameter analysis (far beyond state-of-the-art hospital diagnostics) of the T cell phenotype of COVID-19 patients: months of work from Dr Teresa Prezzemolo, Silke Janssens, Julika Neumann and Dr Mathijs Willemsen. Data analysis by Julika Neumann, Dr Carlos Roca, Dr Oliver Burton and Dr Stephanie Humblet-Baron identified a novel link between IL-10-producing Tregs and COVID-19 severity. We are now following this up to see if the link is useful as a biomarker or even is mechanistic in disease program. We have made our data an open resource (link), allowing other groups around the work to analyse our work. We are continuing to follow these patients and will soon have more and more information about why some patients remain completely healthy and others develop severe, even fatal, disease.
 Dr Dooley and Dr Kouser (pre-COVID-19)We are not just clinical immunologists - we are also basic research immunologists. Mysterious virus triggering immune-mediated destruction of the tissue? We can deal with that. The whole lab contributed to the design of a new potential therapeutic, but I would especially like to call out the contributions of Dr James Dooley, Dr Oliver Burton, Dr Lubna Kouser and Fran Naranjo. Manufacturing is now complete and we are moving to pre-clinical testing. Hopefully we have a vaccine for SARS2 before our treatment is complete, but it is designed to deal with an unknown SARS3 equally well.
Dr Dooley and Dr Kouser (pre-COVID-19)We are not just clinical immunologists - we are also basic research immunologists. Mysterious virus triggering immune-mediated destruction of the tissue? We can deal with that. The whole lab contributed to the design of a new potential therapeutic, but I would especially like to call out the contributions of Dr James Dooley, Dr Oliver Burton, Dr Lubna Kouser and Fran Naranjo. Manufacturing is now complete and we are moving to pre-clinical testing. Hopefully we have a vaccine for SARS2 before our treatment is complete, but it is designed to deal with an unknown SARS3 equally well.
Suffice it to say, we have been as busy as we've ever been, and we will likely remain just as busy well after COVID-19 stops making the headlines. Which brings me to my final plea. Don't forget about scientific research. Unsung heroes during the pandemic, our staff are putting in an enormous effort. And yet we face an incredibly uncertain funding situation. Universities and research institutes have taken an enormous financial blow with this pandemic, and unless governments step in with a large financial rescue package, those scientific research staff who got us through the pandemic are going to be laid off in huge numbers. Even if you don't care about the moral imperative of looking after the people who stepped up when we needed them, there will be a SARS3 or novel flu pandemic in the future. We need to secure the research infrastructure to combat them right now. Science is not a factory that can be switched on and off at will - we need to maintain research excellence, scientific equipment and most of all key staff contracts over the long-term.
 Saturday, May 30, 2020 at 8:45AM
Saturday, May 30, 2020 at 8:45AM As a member of the Liston Lab, I understand
The laboratory is a shared facility with shared space and shared responsibility. As such
Research laboratories can be a place of great stress, making inter-personal relationships intense. When dealing with other members of the laboratory:
 Liston lab
Liston lab  Saturday, May 23, 2020 at 1:01AM
Saturday, May 23, 2020 at 1:01AM 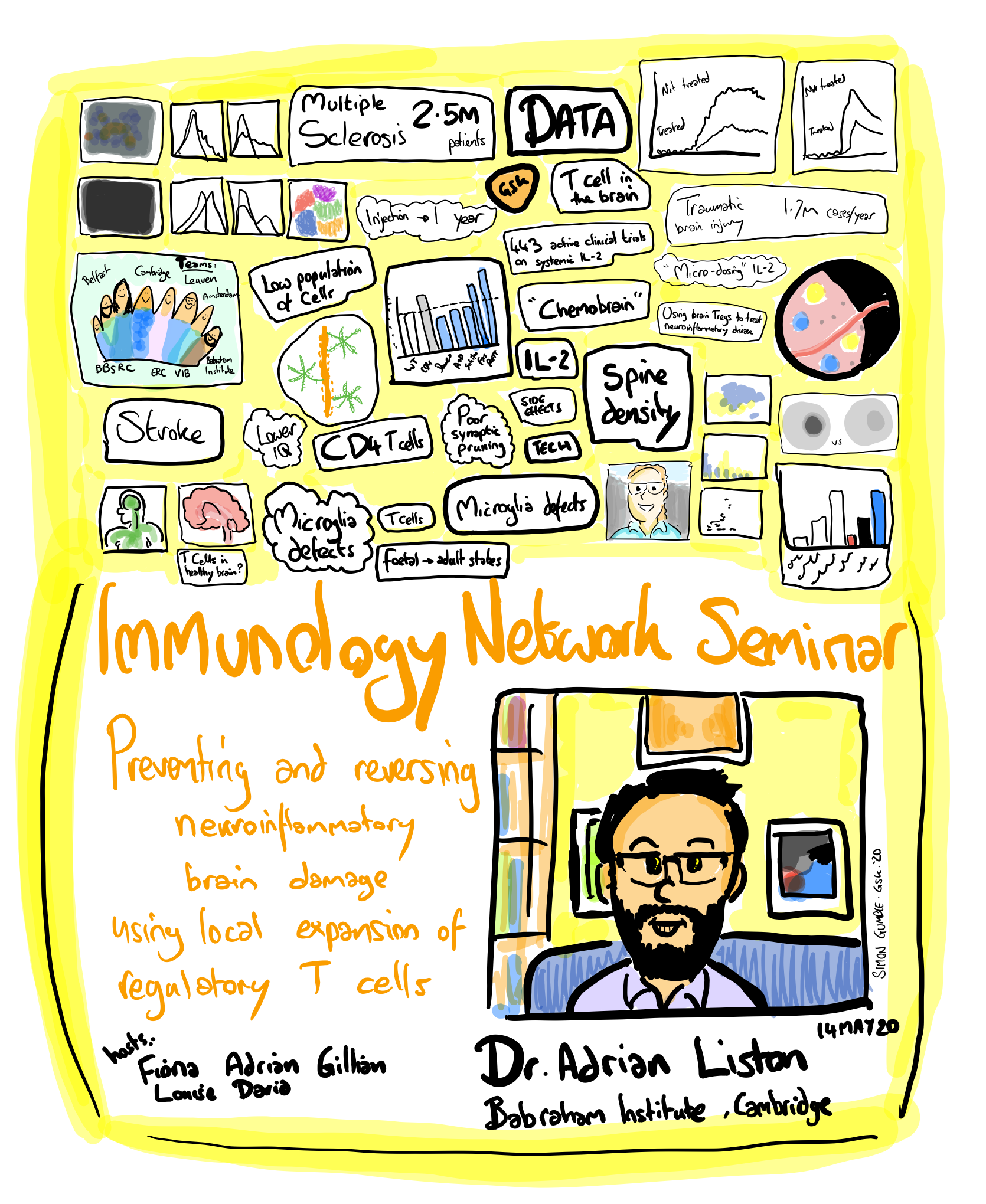
Cartoon courtesy of Simon Gumble, GSK
 Monday, May 18, 2020 at 2:24PM
Monday, May 18, 2020 at 2:24PM This recent twitter thread from a first-gen graduate asking about a PhD got me thinking. As a first-gen graduate myself, what advice would I give to someone starting a PhD? The below is tailored towards a biomed PhD in the UK/EU/Australian systems, but some points are more generalisable:
First, getting into a PhD program is tough. You've made it, congratulations! By definition you have the intellectual ability to finish. Never doubt that. That said, you will doubt it. Especially at the 3-6 month period and at ~2 years in. That is normal. Even though the people around you look confident, they all went through a similar period.
Second, it is your PhD, but the lab's project. You should aim to become the intellectual leader of the project after around a year, but always lead with humility. Others around you will always know more than you on specific techniques or domain knowledge. Being the leader doesn't mean be the boss. It means being the person who makes sure that things are on track, who takes responsibility for keeping up with the literature and following up with people who are part of the team.
Ask for advice, and listen to that advice. Take particular note when it comes from experience. Don't be that student who ignores technicians. When a tech is telling you something, listen. If your supervisor tells you something, listen. Feel free to disagree, but first listen. If someone suggests a protocol for an experiment, do not go back to them for help until you have actually followed their protocol word for word. Don't change protocols that work until you've got a lot more experience. Include every control that is suggested, even the ones you don't think are necessary.
Being a PI is a tough job, very time-demanding. So use their time wisely. Prep before a meeting, take notes during, follow-up. If you can answer a question via a quick google search or conversation with another lab member, do that instead of knocking on their door. A PI can be a valuable asset to you if you use their time wisely. If you start wasting their time they will schedule you out,
The lab environment can be a pressure-cooker of stress. Experiments don't work, trouble-shooting is horrible, publication can be nightmarish. At its best, the shared adversity will create unbreakable bonds between lab members. To make this happen, be considerate, be kind, forgive. Be the team member who helps out. Smile when someone frowns - they may have just had the most horrid day. Soon enough you have a day where you snap or frown - treat them the way you would like to be treated on your worst. Especially keep in mind that science is highly international and multi-cultural, and people may not mean things the way you perceive them (and vice versa).
At the start, get into the lab and learn how it works. Where the tip-boxes go, who refills them and makes up new solutions, how plastics get ordered. Ask the lab manager or senior tech what you can do to help out. There are no magic fairies - every task is done by the team. If you leave the centrifuge messy, use the last reagent without ordering more, you will annoy people. If you clog up their personal pipettes and don't tell anyone, you will really annoy people. Be a good lab citizen.
The first six months is basically you learning how to be in the lab, reading the basic literature and just learning how to do the techniques. You won't actually make any advances - this is all on-the-job training.
Don't hide mistakes. You are going to make mistakes. You are going to make mistakes that will cost your monthly rent's worth in grant money. I remember the horror of breaking a haemocytometer during my first week in the lab. $500 at a time where that was an unbelievable amount of money to me. You make make mistakes that cost your annual salary's worth. Own them. Admit to them. Don't make them again. Never blame others for your mistake. Someone breaking the centrifuge is bad, but if I know they will never do it again I move on. If they blamed someone else for leaving it unbalanced (while they didn't check) then I worry that they haven't taken responsibility and are more likely to make the same expensive mistake again.
You are now the senior PhD student that juniors look at. They see you as calm and capable. You have become a data machine. In about six months you pump out 90% of the data of your PhD. At the same time, you probably see yourself as a bit of a fraud: you know you can handle the day-to-day of the lab, but you doubt you can handle the intellectual side still. Your supervisor now becomes your key asset, probably for the first time, as you start to write up.
Don't spend much time on your first draft, it will be rubbish anyway. Everyone's is. Just write it up and get feedback. Just like any technique, writing is a skill that you will learn, you just have to be willing to give it a shot, get feedback, and try again. This means when you your draft back full of revisions, don't just accept the changes. Try to understand them. What change did you PI make, and could you incorporate that strategy yourself next time? In particular, read papers while writing. Compare your paper to published papers, sentence by sentence to see if your work looks like the real thing. What do figure legends have in your field? Does your draft figure legend have all of these attributes? Remember you are the paper lead, but it is a consensus document. Be generous on coauthorship, and remember who helped you out early on. It means a lot to people to be acknowledged, and it doesn't hurt you to have extra authors on your paper.
 Publication. Ah, this is a horrible ordeal. You will get rejected multiple times, it will feel rubbish. Flip that paper to the next journal and don't take it personally. Don't dwell too much on the comments, the next reviewers may be completely different. If your paper is given a "major revision" - congratulations! That is actually really good news. Now you need to do all the experiments that the reviewers asked that are at all possible. Yes, you could argue the point, but save this for the cases where the experiment is impossible. It is much better to deal with a major revision than to start fresh with a new journal. At the end, you may feel more exhaustion and relief that the paper is off your plate, rather than actual satisfaction. This is (unfortunatey) normal. So make sure you celebrate every intermediate stage (submission, going out to review, major revisions coming back, etc).
Publication. Ah, this is a horrible ordeal. You will get rejected multiple times, it will feel rubbish. Flip that paper to the next journal and don't take it personally. Don't dwell too much on the comments, the next reviewers may be completely different. If your paper is given a "major revision" - congratulations! That is actually really good news. Now you need to do all the experiments that the reviewers asked that are at all possible. Yes, you could argue the point, but save this for the cases where the experiment is impossible. It is much better to deal with a major revision than to start fresh with a new journal. At the end, you may feel more exhaustion and relief that the paper is off your plate, rather than actual satisfaction. This is (unfortunatey) normal. So make sure you celebrate every intermediate stage (submission, going out to review, major revisions coming back, etc).
Remember you don't actually need to publish to graduate (in the UK or Australia, in much of the EU you do, but there is a journal home for every paper). You just need to produce a body of work suitable for publication. Like your paper, just push out the first thesis draft quick and dirty. It is a formality, nothing more. Your contribution is in your papers, while your thesis will be read by the jury only, and then gather dust on the shelves somewhere.
Congratulations! You have a PhD. The highest degree possible. You are now an expert in your chosen field (although we all have more to learn!). You have many, many good career options available to you. A PhD in biomedical sciences is a gateway to so many interesting careers. Go down a pathway that looks interesting to you, and if it doesn't work out, pick a new path. The world is your oyster!
 science careers
science careers  Thursday, April 23, 2020 at 7:01PM
Thursday, April 23, 2020 at 7:01PM Severe congenital neutropenia leaves young patients to contract infection after infection, leading to life-threatening situations. A team of Leuven scientists has identified a novel genetic mutation, pointing to a new causative mechanism for this severe immune disorder.
The story starts with patient Jane Doe, now 19 years old, but diagnosed with severe congenital neutropenia when she was just 2 years old. By that time, she had already suffered an ear abscess, recurring ear infections, bronchitis, sinusitis, tonsillitis and several gum infections.
 After yet another infection, this time of her intestine, a detailed investigation revealed a striking shortage of neutrophils, white blood cells that are recruited as first-responders to the site of injury or infection within our body. Having an abnormally low concentration of neutrophils in the blood is referred to as neutropenia. When it is severe and present from birth (congenital), that is where the diagnosis of severe congenital neutropenia comes in.
After yet another infection, this time of her intestine, a detailed investigation revealed a striking shortage of neutrophils, white blood cells that are recruited as first-responders to the site of injury or infection within our body. Having an abnormally low concentration of neutrophils in the blood is referred to as neutropenia. When it is severe and present from birth (congenital), that is where the diagnosis of severe congenital neutropenia comes in.
“Severe congenital neutropenia is very scary, because these kids develop serious infections that can be lethal for infants,” explains Erika Van Nieuwenhove. “As if that’s not enough, they are also at increased risk for other conditions such as leukemia.”
Van Nieuwenhove is both an MD and PhD, who combines clinical work in the university hospital with Carine Wouters, with research at VIB and KU Leuven under the guidance of Adrian Liston and Stephanie Humblet-Baron.
Together with John Barber and several other colleagues, she set out to understand why Jane Doe developed SCN in the first place. Van Nieuwenhove: “For up to 50% of severe congenital neutropenia patients, we have no clue what causes the disease. It was the same for our patient, whose parents are both healthy.”
A new mutation in a familiar gene
After Jane Doe tested negative for mutations in all the genes with known ties to neutropenia, the researchers performed whole exome sequencing, probing every gene in the DNA, to trace back the genetic defect underlying the disorder.
“We identified a new mutation in a gene called SEC61A1, which encodes one of three subunits of the Sec61 complex. This molecular complex plays a crucial role in both protein transport and in maintaining the calcium balance of the cell,” explains Humblet-Baron. “Our experiments revealed that the genetic defect led to both a lower expression and a reduced efficacy of the SEC61A1 protein, and that these quantitative and qualitative defects in turn disturb neutrophil differentiation and maturation.”
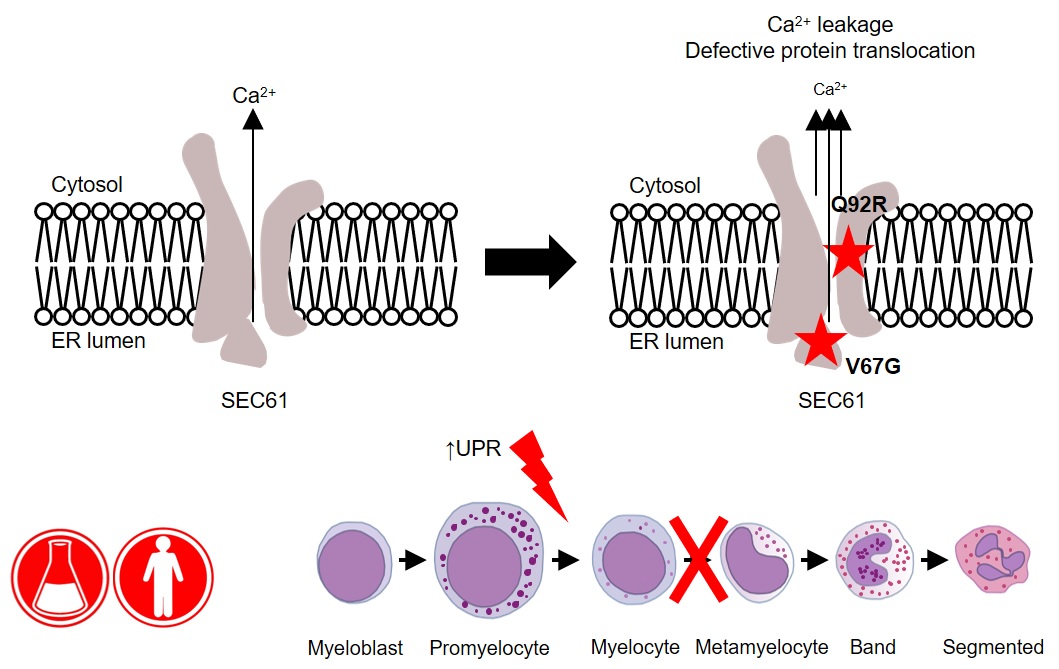
Interestingly, SEC61A1 has recently been picked up in other studies that were not focused on neutropenia. Different mutations in the same gene were reported in two families with a rare kidney disease and in two additional families with an antibody deficiency.
“The fact that there are different mutations in the same gene indicates there may be overlapping mechanisms among the different disorders. With the low number of currently known patients, it is still too early to predict which mutations can lead to which symptoms,” explains Liston.
“What’s clear from our findings is that SEC61A1 mutations can also cause severe congenital neutropenia. Considering this gene’s link with other disorders, the clinical implications of our work reach far beyond the patient with whom it all started here in Leuven.”
—
Read the original paper: Defective SEC61α1 underlies a novel cause of autosomal dominant severe congenital neutropenia. Van Nieuwenhove et al. JACI 2020
 Thursday, April 23, 2020 at 6:49PM
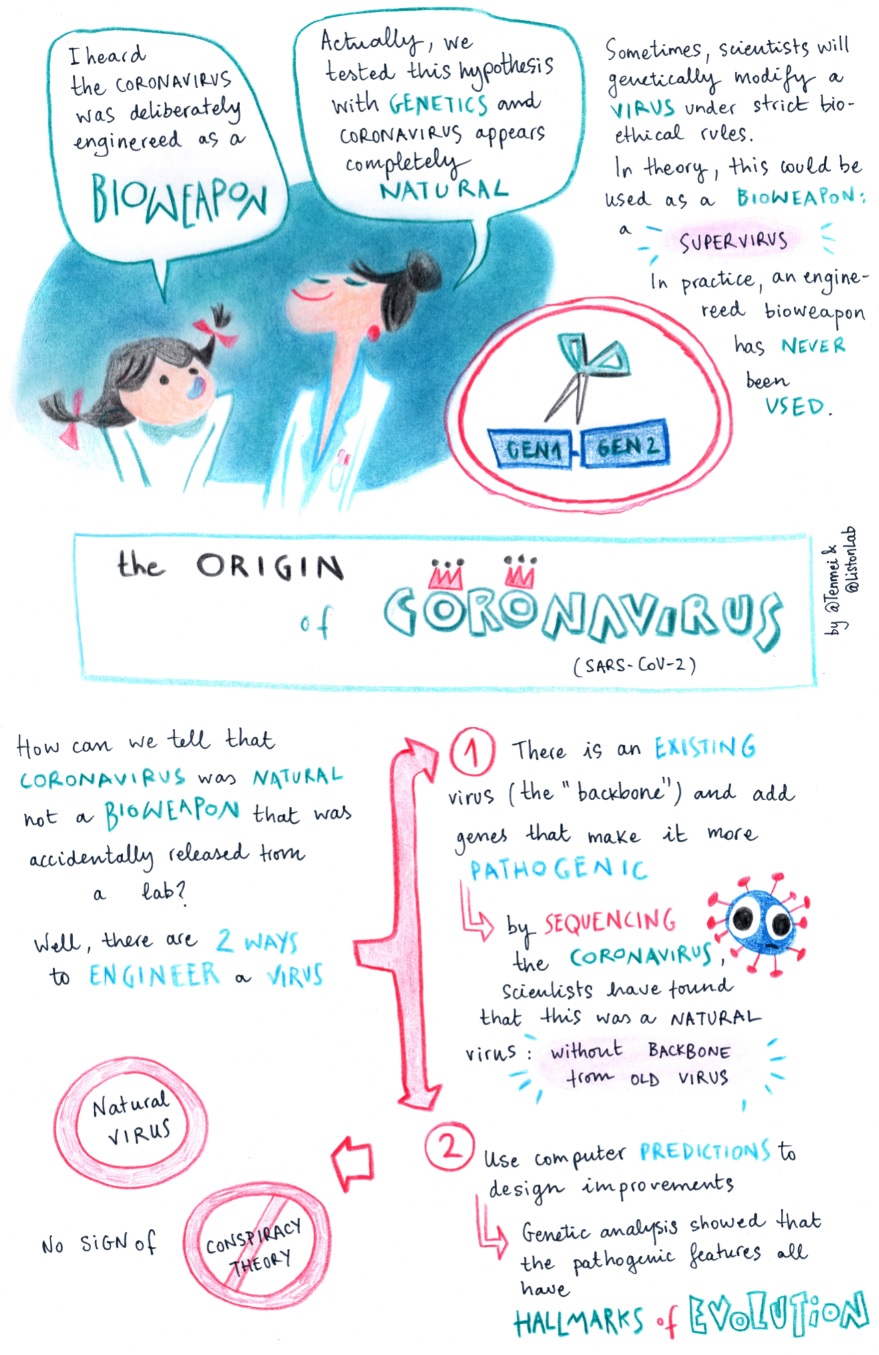
Thursday, April 23, 2020 at 6:49PM Coronavirus science simplified: number 5. This article in Nature Medicine used genetic analysis to test the hypothesis that SARS-CoV-2 was generated in a lab as a bioweapon. Spoiler alert: it wasn't. Clear hallmarks of natural evolution and none of the features of a designed virus. Read the original paper, or see the illustrated abstract by Tenmai.
 Thursday, April 16, 2020 at 12:17PM
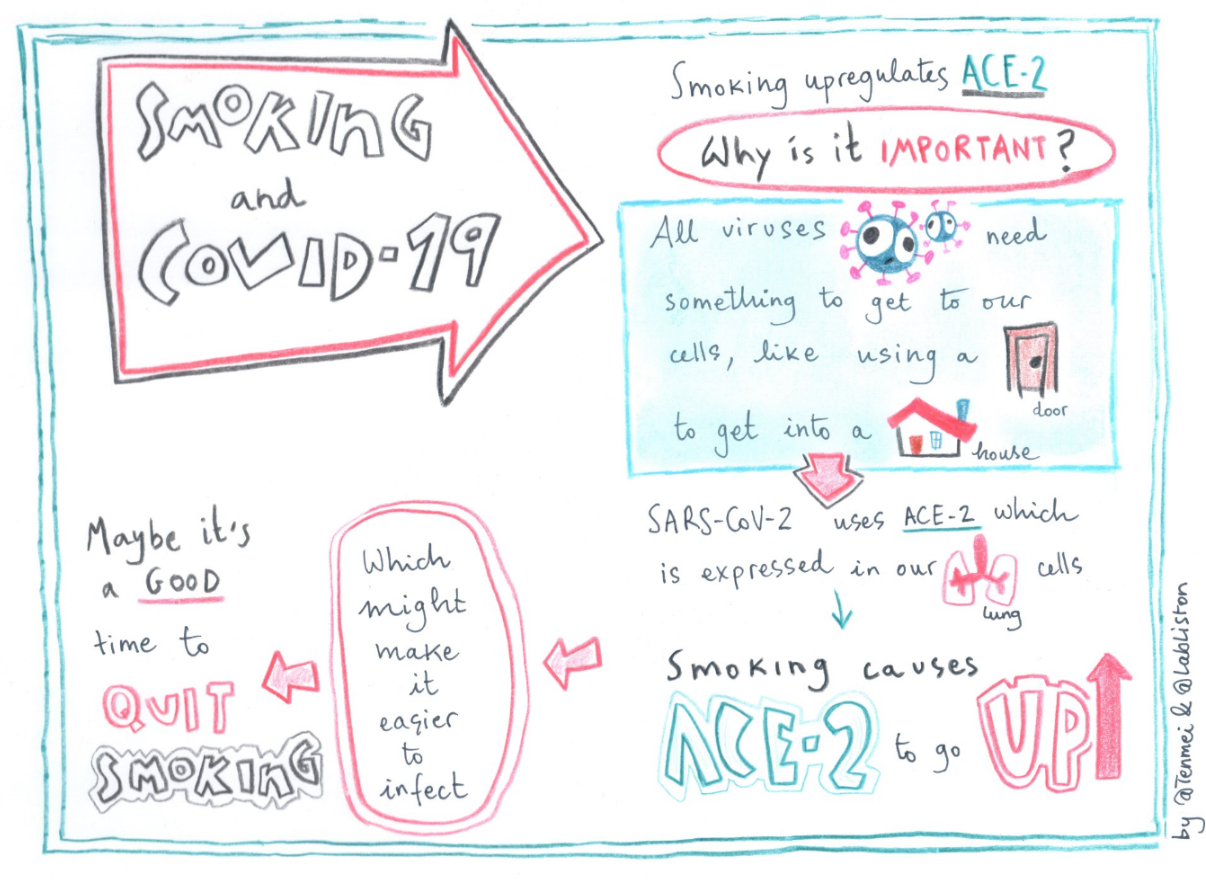
Thursday, April 16, 2020 at 12:17PM "Coronavirus science simplified" edition 4. This paper looks at the expression of the protein ACE2 in smokers and ex-smokers. Why is this important? Read the pre-print (like a scientific paper, but it hasn't been reviewed yet - consider it a preliminary result), or see the illustrated abstract from TenMei:
 Wednesday, April 15, 2020 at 11:40AM
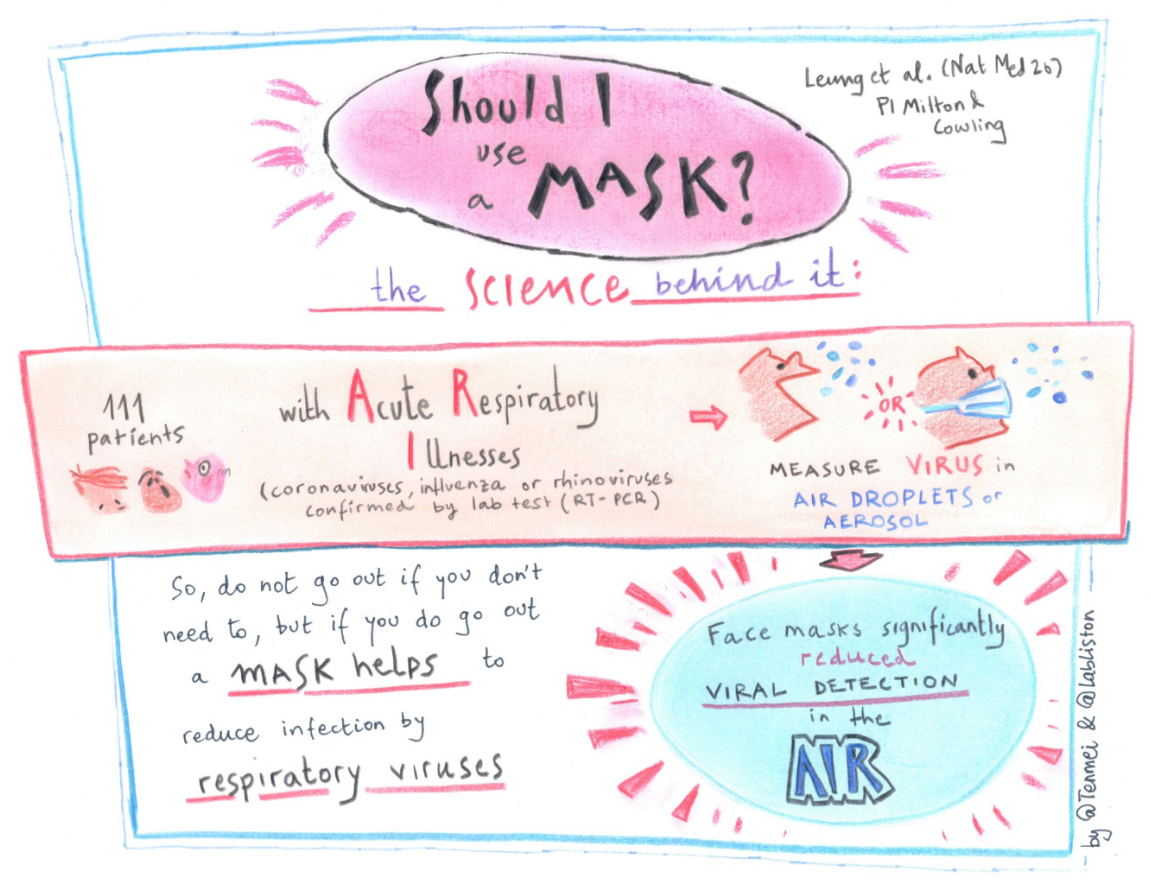
Wednesday, April 15, 2020 at 11:40AM The third paper in our series on "Coronavirus science simplified". The talented TenMei is taking cutting-edge papers on Coronavirus and boiling them down to an illustrated abstract. Today's paper is "Respiratory virus shedding in exhaled breath and efficacy of face mask". You can read the original here, with the key message simplified: