Responding to the COVID crisis
 Friday, December 3, 2021 at 5:23PM
Friday, December 3, 2021 at 5:23PM As well as exposing weaknesses in healthcare systems and supply chains, the coronavirus pandemic has underscored the importance of fundamental research and collective effort. During 2020, scientists rose to the challenge of developing new vaccines and effective treatments for Covid-19. Institute immunologists Dr Michelle Linterman and Professor Adrian Liston describe how their labs responded and the lessons we must learn.
In the early days of the coronavirus pandemic, as lockdowns loomed, workplaces closed and travel slowed to a trickle, Dr Michelle Linterman was certain of one thing – she wanted to make her group’s expertise available to the global vaccines effort.
Among those working on a vaccine against SARS-CoV-2 (the coronavirus that causes Covid-19) was Dr Teresa Lambe at the Jenner Institute in Oxford. “I already knew Tess, so once it became clear they had a vaccine candidate, my first instinct was to ask her what we could do to help,” Linterman recalls.
As an immunologist, Linterman’s work focuses on how the immune system responds to vaccines. In particular, she wants to understand why older people respond less well to vaccines, something she studies using human vaccination studies and in aged mice. “I thought the most useful thing was for us to offer something that nobody else could contribute quickly – and that was our ability to use aged mice as a pre-clinical test of how this vaccine is likely to work in an ageing immune system,” she says.
When Lambe said yes, Linterman set up trials to compare immunological responses to the Oxford/AstraZeneca vaccine in young and aged mice, and discovered that although aged mice responded more poorly than young mice to a single dose, after two doses of the vaccine, the immune responses were very good in both groups.
The study helped both institutes. For the Jenner, it showed two doses of the vaccine would give good protection against infection in all adults. For Babraham, it provided new insights into vaccine responses at a cellular and molecular level, expanded research into new vaccine platforms and led to new collaborations. Most importantly, it illustrated the value of publicly-funded research.
“Because we’re funded by the BBSRC – in other words the tax payer – it was incredibly important to use our knowledge and expertise to contribute to vaccine development in the midst of the pandemic,” she says.
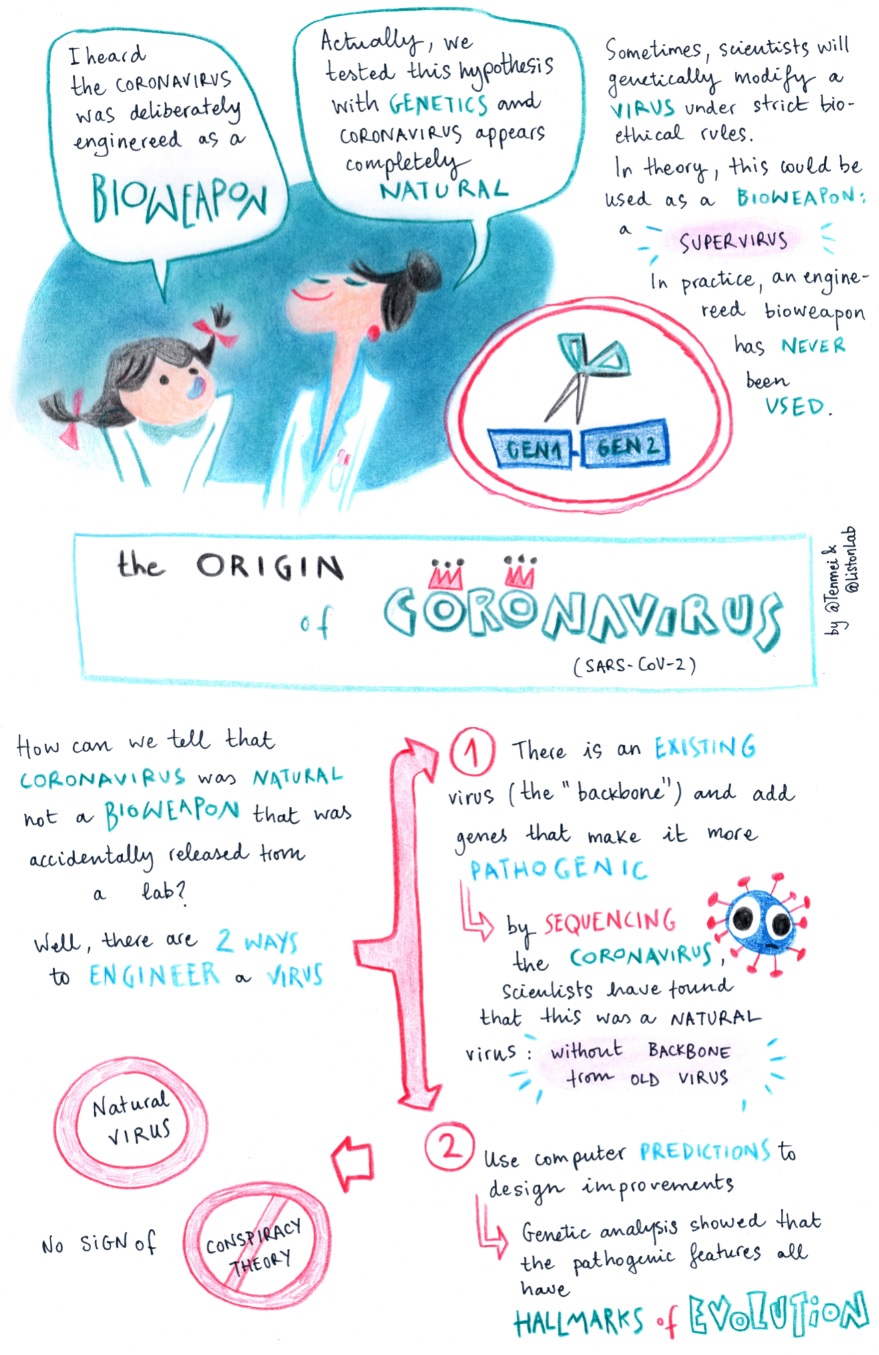
Fellow immunologist Professor Adrian Liston also stepped up to the mark, using his research to help clinicians make the best treatment choices for Covid-19 patients and his communication skills to provide accurate information to journalists and the public.
“We need to develop good systems for treating emerging viruses before we know much about them, which is something my lab is working on,” explains Liston. “We are coming up with treatments that are vaccine agnostic, treatments that will work for most viruses with the potential to become pandemic, regardless of the actual virus.”
Liston’s group is also interested in systems immunology – exploring what makes people’s immune systems so different from each other.
This variation has been graphically illustrated during the pandemic, some people experiencing mild symptoms while others died. “Diversity is intrinsically important to the immune system. It’s the most genetically-diverse system in the human body, and there are other factors at play, such as age, gender and weight,” he explains.
Being so close to events has taught Liston and Linterman many lessons – lessons, they say, that are vital for political leaders to learn. First, zoonoses (diseases spread between animals and humans) with pandemic potential are far from rare events. “They occur every couple of years,” says Liston. “We’ve had coronavirus outbreaks before, like SARS and MERS; they happen like clockwork. In the previous outbreaks we had better luck and better preparation. These are things we must prepare for.”
Secondly, we must guard against complacency. “If we pat each other on the back for a job well done, and then slash science budgets, the next outbreak will be as bad as this one,” he warns. “We must fund surveillance as well as immunology and virology research, because if you scale down this science it takes a decade or more to rebuild that intellectual capital.” This preparation extends to supporting fundamental research in a broad range of areas. “We need to fund fundamental research because you’re never sure which bit of it will save you in the future,” says Linterman.
Third, a global approach to research, and funding to support this, is essential, because scientific discoveries are not bounded by borders, adds Linterman: “One of the reasons the Oxford vaccine was developed so fast was because of years of work on Ebola and MERS using the same adenoviral vaccine vector.”
As vaccines are rolled out, and countries emerge from lockdown, we might usefully reflect on what we would have done without a vaccine. It’s a scenario that frightens Linterman. “There wasn’t another exit strategy,” she says. “The vaccines are great, far better than we expected. But there are pathogens that we don’t have good vaccines for. For me, that’s the scary thing. We’re lucky the vaccines are so effective – but that doesn’t mean the same will be true for the next pandemic.”
This feature was written by Becky Allen for the Annual Research Report 2019-2020.
 Coronvavirus,
Coronvavirus,  Liston lab
Liston lab