Research using mice and human data shows how diet affects disease risk
Eating a diet high in sugar increases the likelihood of developing pancreatic cancer in some individuals and also drives the aggressive growth of tumours, a study by researchers from the Babraham Institute, Cambridge, UK, and VIB-KU Leuven, Belgium, has found.
 The researchers completed a comprehensive project using experimental work in mice and human data, including from pancreatic cancer patients, to understand the influence of different dietary components on the development and progression of pancreatic cancer. The research is published today in the journal Cell Reports.
The researchers completed a comprehensive project using experimental work in mice and human data, including from pancreatic cancer patients, to understand the influence of different dietary components on the development and progression of pancreatic cancer. The research is published today in the journal Cell Reports.
Pancreatic cancer is a rare but fatal form of cancer, due to late detection and a poor understanding of the risk factors. Known risk factors include obesity, diet and type 2 diabetes, however the low incidence rate and interconnection of these factors mean that it is difficult to tease apart their individual contribution.
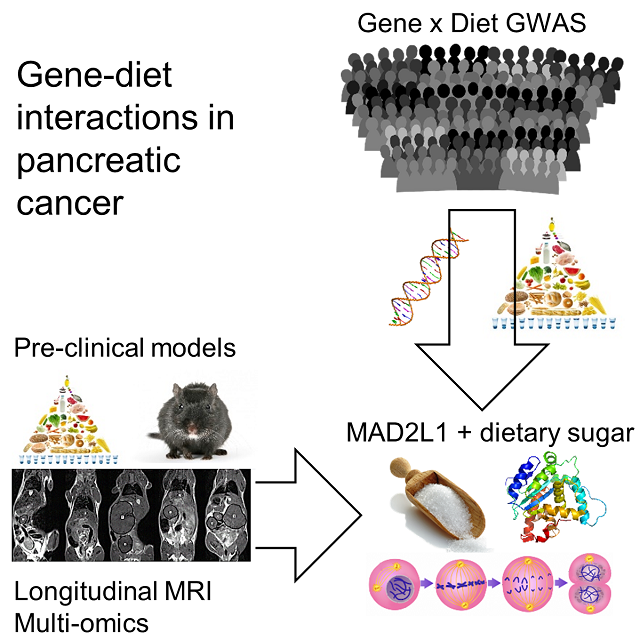
The researchers first studied the effects of obesity, diet and diabetes on pancreatic cancer development, growth and lethality in mice. In parallel they analysed the effect of diet using data from the European Prospective Investigation into Cancer and Nutrition (EPIC) study, which followed over half a million Europeans for 20 years.
The researchers found that obesity, diet and diabetes had profound and differing impacts on cancer incidence and growth. Using mice, the results indicated that obesity, dietary animal fats and dietary sugar were independent drivers of different facets of pancreatic cancer progression. In particular the results shed light on how pancreatic cancer might be affected by dietary sugar, with more rapid tumour growth and escalated lethality.

The effect of dietary sugars on pancreatic cancer development was preserved between mice and humans. In 500 study participants with pancreatic cancer, the researchers explored the interaction between genes and diet and found that high levels of dietary sugar increased pancreatic cancer risk in individuals with a certain genetic variation (found in 6% of the population).
 Dr James DooleyDr James Dooley, senior staff scientist in the Immunology programme at the Babraham Institute, said: "Our study raises concern about the remarkable toxicity of sugar in our diet. We spent years looking at different dietary and genetic changes, and nothing has anywhere near the detrimental impact of a high sugar diet. Our findings suggest that it drives pancreatic cancer onset and makes it a more aggressive and lethal tumour."
Dr James DooleyDr James Dooley, senior staff scientist in the Immunology programme at the Babraham Institute, said: "Our study raises concern about the remarkable toxicity of sugar in our diet. We spent years looking at different dietary and genetic changes, and nothing has anywhere near the detrimental impact of a high sugar diet. Our findings suggest that it drives pancreatic cancer onset and makes it a more aggressive and lethal tumour."
Analysis of the human-derived data from the large EPIC study suggested that dietary plant fats reduced the risk of pancreatic cancer, estimating a 10% decrease in risk when eating the equivalent of an avocado a day.
Professor Adrian Liston, senior group leader at the Babraham Institute, said: "This study shows the power of combining animal research with the study of patients. We were able to use epidemiology and large patient-based resources to find a link in humans, and then go back to an animal model to formally test the direction of causality. Finding the same gene-diet link in both mice and humans makes us confident that diet is modifying disease risk, and gives us the tools to test preventative and therapeutic interventions."
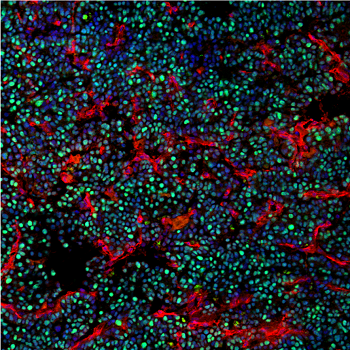
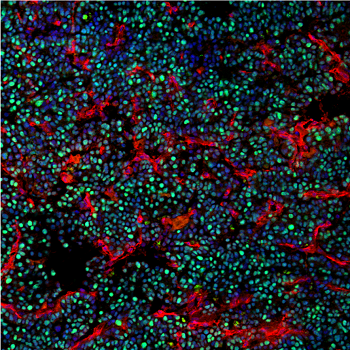 Proliferating pancreatic cancer cells in mice fed high sugar dietsWhile the impact of nutrition on cancer development continues to be explored and debated, this study provides a vital foundation for further studies and important indications to explore. Armed with this knowledge, clinicians could be supported to identify individuals at increased risk for screening and individuals with a high-risk genetic background could take pro-active dietary changes to reduce their risk of pancreatic cancer.
Proliferating pancreatic cancer cells in mice fed high sugar dietsWhile the impact of nutrition on cancer development continues to be explored and debated, this study provides a vital foundation for further studies and important indications to explore. Armed with this knowledge, clinicians could be supported to identify individuals at increased risk for screening and individuals with a high-risk genetic background could take pro-active dietary changes to reduce their risk of pancreatic cancer.
Ali Stunt FRSA, Founder and Chief Executive of Pancreatic Cancer Action, concurs: "Here at Pancreatic Cancer Action, we strongly advocate for high quality research into this neglected cancer. Dr Liston and his team have made a major contribution into understanding how diet and genetics changes the risk for pancreatic cancer. Healthy lifestyle choices, such as avoiding sugar-sweetened beverages and choosing a diet rich in vegetables, can reduce your risk of pancreatic cancer, and may be especially important in families with a history of the disease."
Read the original article here.
 Tuesday, July 28, 2020 at 7:22PM
Tuesday, July 28, 2020 at 7:22PM  Liston lab,
Liston lab,  cancer,
cancer,  metabolism
metabolism